From the Annals of Gastroenterology, Marilia Carabotti et al, 2015 Apr-Jun; 28(2): 203–209
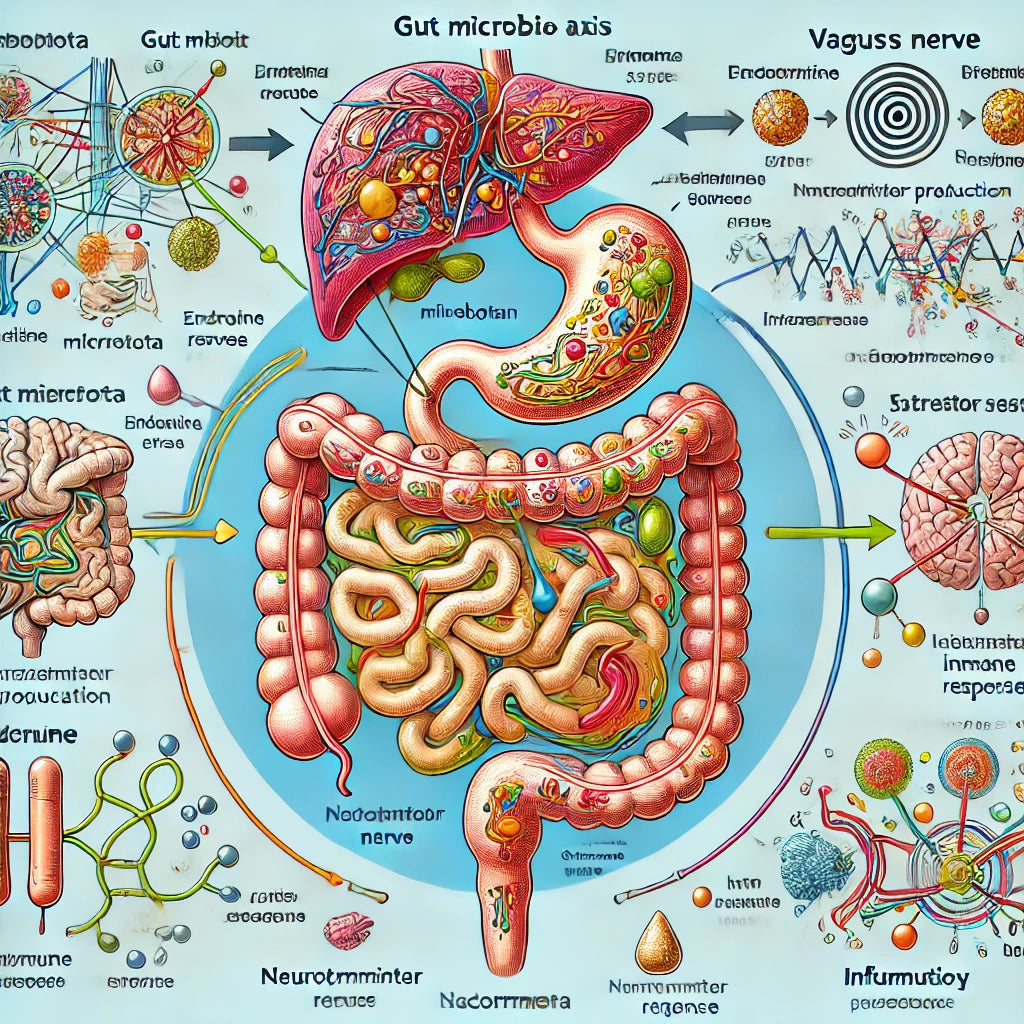
The research paper titled "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems" explores the bidirectional communication between the gut microbiota and the brain. The gut-brain axis (GBA) links emotional and cognitive centers of the brain with peripheral intestinal functions through neural, endocrine, immune, and humoral pathways. The study highlights the role of gut microbiota in influencing these interactions and suggests that alterations in microbiota composition can impact conditions like autism, anxiety, depression, and irritable bowel syndrome (IBS). It also discusses how microbiota can affect brain chemistry, stress responses, and cognitive functions, suggesting potential therapeutic roles for probiotics and diet in treating neurologic and gastrointestinal disorders. The paper emphasizes the importance of a balanced gut microbiota for maintaining gut and brain health.
From the Journal Integrated Medicine, Jeremy Appleton, 2018 Aug; 17(4): 28–32
The research paper titled "The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health" explores the complex bidirectional communication between the gut microbiota and the brain. The gut-brain axis (GBA) includes neural, endocrine, humoral, and immune pathways, highlighting the extensive influence of gut microbiota on mental health.
Key Points:
Gut-Brain Axis (GBA) Overview: The GBA links the enteric nervous system (ENS) and central nervous system (CNS). This communication is facilitated through the autonomic nervous system, the hypothalamic-pituitary-adrenal (HPA) axis, and gut-based neural pathways.
Impact of Gut Microbiota on Mental Health: Research indicates that gut microbiota profoundly affects mood, cognition, and mental health. Fluctuations in microbiota composition have been linked to mood disorders such as anxiety, depression, and autism spectrum disorders (ASD). Additionally, gastrointestinal diseases like irritable bowel syndrome (IBS) often co-occur with psychological comorbidities.
Mechanisms of Microbiota Influence:
Neurologic Pathway: The vagus nerve and neurotransmitters like GABA, serotonin, and histamine are key players. Gut bacteria can produce these neurotransmitters, influencing brain chemistry and behavior.
Endocrine Pathway: Gut microbiota affects the release of biologically active peptides from enteroendocrine cells, impacting the HPA axis and stress responses.
Humoral/Metabolic Pathway: Metabolites like short-chain fatty acids (SCFAs) produced by gut bacteria have hormone-like activities and can cross the blood-brain barrier, influencing brain development and behavior.
Immune Pathway: Gut microbiota interacts with the immune system, influencing the release of cytokines and other mediators. Dysbiosis can trigger inflammatory responses that affect the CNS.
Clinical and Preclinical Research:
Animal studies have shown that gut bacteria can influence stress responses, brain plasticity, and behavior.
Human studies have investigated the use of probiotics to manage conditions like depression and anxiety, with varying results. Certain probiotics have shown promise in reducing symptoms of depression and anxiety, suggesting potential therapeutic applications.
Influence of Diet: Diet plays a significant role in shaping gut microbiota and, consequently, its impact on mental health. Nutritional interventions can potentially modulate gut microbiota to improve cognitive function and mental well-being.
Potential Therapeutics: The concept of "psychobiotics" has emerged, referring to probiotics that have a beneficial effect on mental health. Clinical trials are ongoing to validate their efficacy and establish guidelines for their use.
Conclusion:
The paper emphasizes the crucial role of gut microbiota in maintaining mental health through the gut-brain axis. Understanding these interactions opens new avenues for treating psychiatric and gastrointestinal disorders, highlighting the potential of diet and probiotics as therapeutic tools.
From Annual Review of Medicine, Emeran A. Mayer et al, vol 73, 2022
The research review titled "The Gut–Brain Axis" from Annual Reviews provides a comprehensive analysis of the bidirectional interactions among the brain, gut, and gut microbiome, which are crucial in regulating various physiological and homeostatic functions. Here are the key points summarized from the research:
Bidirectional Communication: The gut-brain axis involves complex, nonlinear communication channels with multiple feedback loops, integrating signals between the brain, gut, and microbiome.
Pathophysiology and Disorders: Alterations in gut-brain-microbiome interactions have been identified in several digestive, psychiatric, and neurological disorders. However, a clear causative role of the microbiome in conditions like irritable bowel syndrome (IBS) remains undetermined.
Microbiome and Brain Disorders: Recent studies suggest that the microbiome may influence psychiatric and neurological disorders such as depression, anxiety, Alzheimer's disease, Parkinson's disease, and autism spectrum disorder, shifting the understanding of these conditions beyond solely brain-related mechanisms.
Interoception: The ability of the brain to sense and process internal physiological states, known as interoception, is influenced by gut microbes and their metabolites. This interaction plays a crucial role in maintaining homeostasis and influencing motivational states, emotional reactions, and homeostatic reflexes.
Signaling Molecules: Gut microbes produce various signaling molecules, including short-chain fatty acids (SCFAs) from dietary fibers, which affect neuroplasticity, gene expression, food intake, and immune system modulation. Other important molecules include metabolites from tryptophan, bile acids, and estrogen, which are influenced by gut microbes and play significant roles in physiological processes and disease mechanisms.
Barriers to Signaling: The intestinal barrier and the blood-brain barrier are crucial in modulating gut-brain-microbiome signaling. Factors like diet, stress, and inflammation can affect the permeability of these barriers, influencing the overall communication and health of the system.
Therapeutic Approaches: Current therapies for disorders like IBS focus on dietary interventions (e.g., low-FODMAP diet), cognitive-behavioral therapy (CBT), and pharmacological treatments targeting the gut-brain-microbiome system. However, the effectiveness of these treatments varies, and more well-designed randomized controlled trials are needed to establish their efficacy.
Future Directions: The research highlights the need for personalized microbiome-targeted therapies and a better understanding of the gut-brain-microbiome interactions to develop effective treatments for related disorders.
The review emphasizes the intricate and dynamic nature of the gut-brain axis and its significant impact on health and disease, pointing towards the potential of microbiome-targeted therapies in the future.